Heart Failure
Heart failure means your heart isn’t able to pump enough blood to the rest of your body.
How does a healthy heart work?
What is heart failure?
What are the causes of heart failure?
What are the signs and symptoms of heart failure?
What are the possible tests to diagnose heart failure?
What are the possible treatments for heart failure?
What is the future plan if you have heart failure?
How does a healthy heart work?
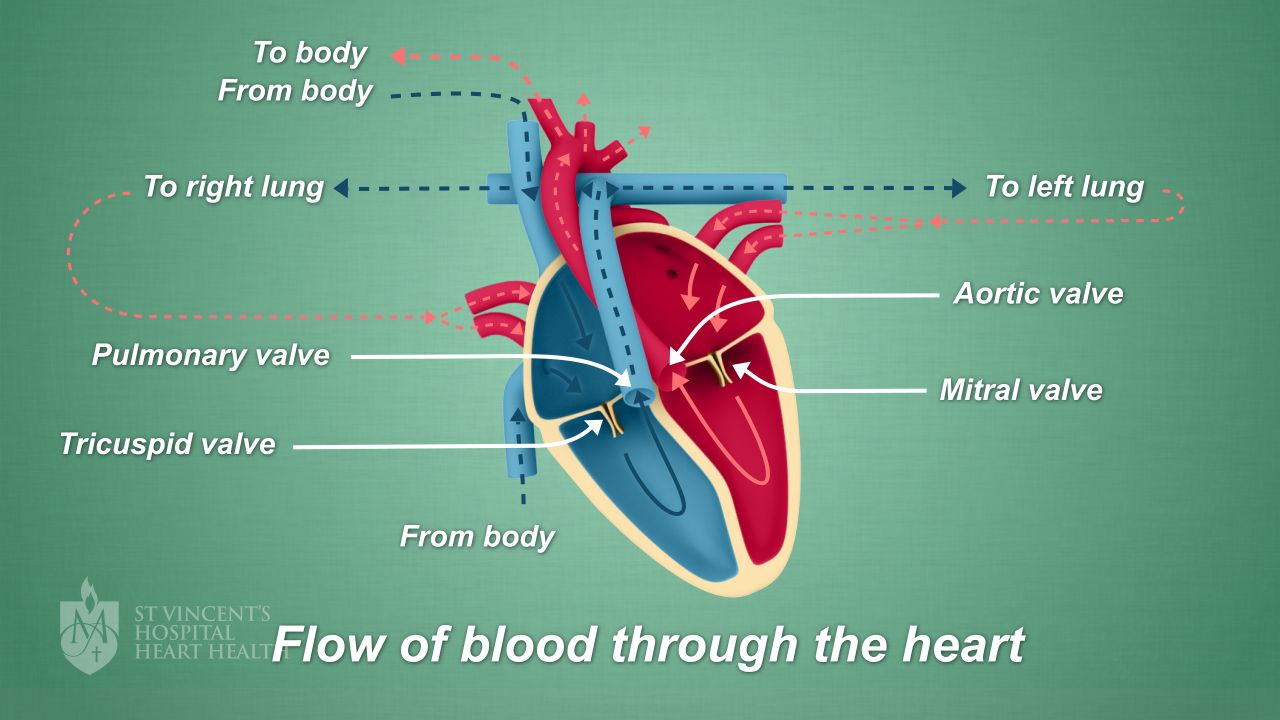
Your heart is a truly amazing organ. It works like a pump, giving your body a steady supply of oxygen-rich blood. Blood flows in and out of your heart in a cycle.
This image below shows how the blood flows through your heart.
What is heart failure?
Heart failure doesn’t mean your heart has failed or stopped working. It really means your heart isn’t able to pump enough blood to the rest of your body. This could happen because your heart has become larger or thicker - and as a result, it isn't able to squeeze or relax properly.
What are the causes of heart failure?
The most common causes of heart failure are:
What are the signs and symptoms of heart failure?
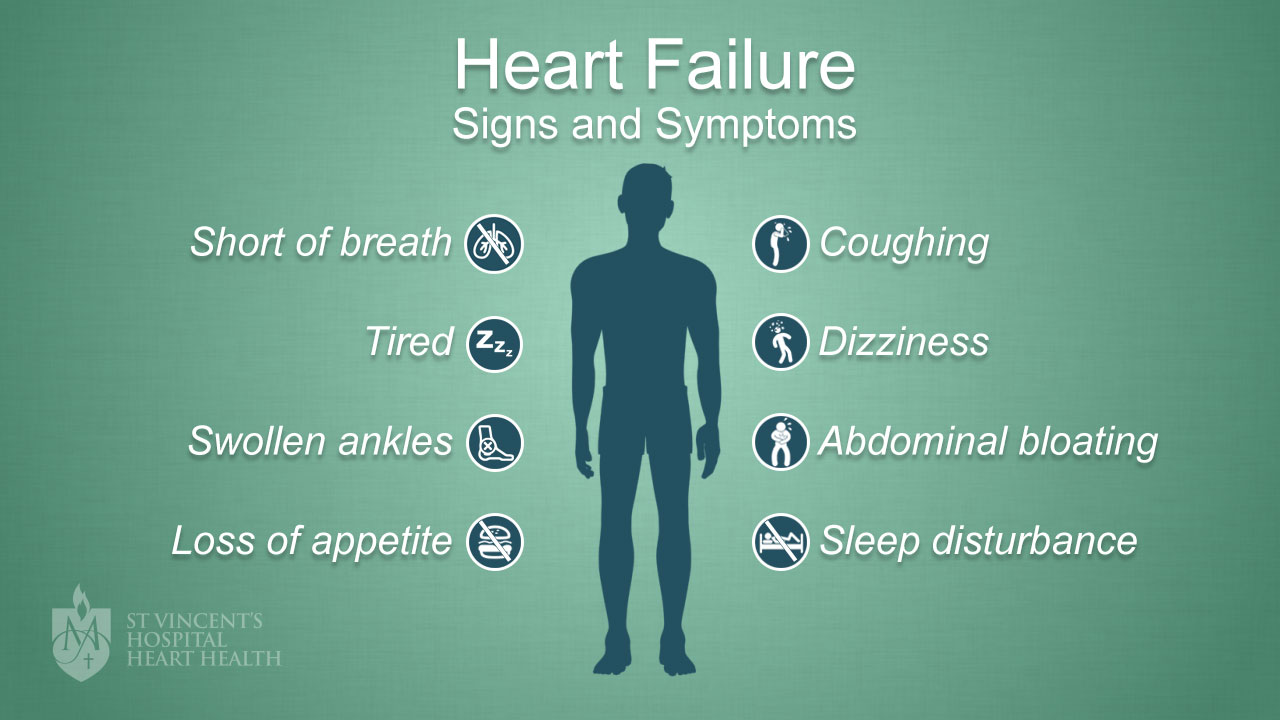
Heart failure can cause symptoms, but not everyone will experience all of them.
The most common symptom of heart failure is feeling short of breath - either with rest or exercise. Tiredness and swollen ankles are also very common. Coughing - particularly at night - as well as bloating in the abdomen, dizziness, sleep disturbance, and loss of appetite are all symptoms that people with heart failure can feel.
Each of these symptoms are shown in the diagram below:
What are the possible tests to diagnose heart failure?
It’s important to have the appropriate tests to determine if heart failure is the cause of your symptoms. Your doctor will ask you about your symptoms and your medical history, and complete an examination of your heart and lungs, before ordering tests. The results of your tests will tell your medical team if you have any underlying problems that may affect your heart.
You may need one or more of the following tests:
- Chest X-ray – to check your heart’s size and find out if there’s any fluid in your lungs
- Echocardiogram – a simple test using ultrasound waves to look at how your heart pumps blood, check your blood flow and see how well your heart’s valves are working
- ECG – an electrical recording of your heart’s action
- Blood tests – to check how your other organs are responding, such as your kidneys and liver
- Coronary angiogram – to check your blood flow through your coronary arteries. These are the fuel lines that carry blood to the heart muscle
There are other tests that may be required, and your doctor will discuss these with you. Your doctor may also consider ordering tests for other types of conditions which can cause the same symptoms as heart failure.
What are the possible treatments for heart failure?
If you’re diagnosed with heart failure, don’t be alarmed. There are many treatments that can help and plenty of support available to help you manage your condition. Your heart failure team will work with you to develop a personalised treatment plan.
The aim of your treatment will be to improve your symptoms and quality of life, improve your heart function, and treat any underlying causes of your heart failure.
Your team will consist of specialists (nurse, pharmacist, physio, and dietitian) who can help you to treat and manage your symptoms and lifestyle changes in hospital and at home. There are many steps you can take now to start improving your symptoms:
- Quitting smoking – your nurse, pharmacist or doctor can support you by suggesting nicotine replacement therapy or refer you to Quitline
- Limiting the amount of fluid you drink – aim for no more than 1.5 litres (6 cups) of fluid, (eg water, tea, juice, coffee). You can print a fluid balance chart to help you keep a record of how much you are drinking
- Reduce your salt intake – too much salt in your diet can cause fluid retention and put strain on your heart
- Weigh yourself daily – monitor yourself for signs of increased fluid in the body (and report any sudden increase of 2kg in 2 days to your doctor)
- Monitor yourself daily for symptoms of fluid retention – symptoms can include increased shortness of breath or ankle swelling
- Get your annual flu vaccination – the flu shot helps to prevent chest infections which can worsen your heart failure symptoms
- Reduce your alcohol intake – alcohol can cause heart failure in some people, so talk to your doctor about safe drinking
- Exercise regularly – exercising can help to improve your general wellbeing and heart function – talk to your doctor about starting an exercise program
- Medications - heart failure medications are designed to improve your symptoms as well as increase your life expectancy. The medications prescribed for you will depend on your type of heart failure and any other health problems you may have. It’s likely you’ll need several types of medication and the doses may need to be changed from time to time
Other treatments that might help to improve your heart failure symptoms include pacemaker surgery and different types of heart surgery, including heart bypass surgery and valve surgery. Your doctor will recommend these if your medical team feel they will be helpful for you.
What is the future plan if you have heart failure?
Heart failure is a serious condition, yet just like diabetes or asthma, it can be managed. As you plan for the future, one of the most important things you can do is stay positive. There are many options to help you if you’ve been diagnosed with heart failure, and your GP and heart failure nurse will support you every step of the way.
You’ll be given guidance and instructions on how to manage your condition and live a healthy life, including:
- Following your dedicated treatment plan – always take your medicines, continue to make healthy lifestyle changes, stay active, and go to your regular medical appointments
- Knowing when to seek help – if something doesn’t feel right, always contact your doctor or heart failure nurse.
- See a dedicated cardiac rehabilitation or heart failure service or nurse – your medical team can help to arrange extra support or care at home, and you can also see dedicated community heart failure nurses (ask your doctor for a referral)
- St Vincent’s Hospital Heart Failure Service – a home visiting team of health professionals can teach you about how to best manage your heart failure and monitor your condition