Cardiomyopathy
Cardiomyopathy is a disease which causes the heart muscle to become bigger, thicker or stiff.
What is cardiomyopathy?
What are the causes of cardiomyopathy?
What are the signs and symptoms of cardiomyopathy?
What are the possible tests to diagnose cardiomyopathy?
What are the possible treatments for cardiomyopathy?
What is the future plan if you have cardiomyopathy?
What is cardiomyopathy?
Cardiomyopathy is a disease that affects the way that the heart muscle pumps. Some types of cardiomyopathies are:
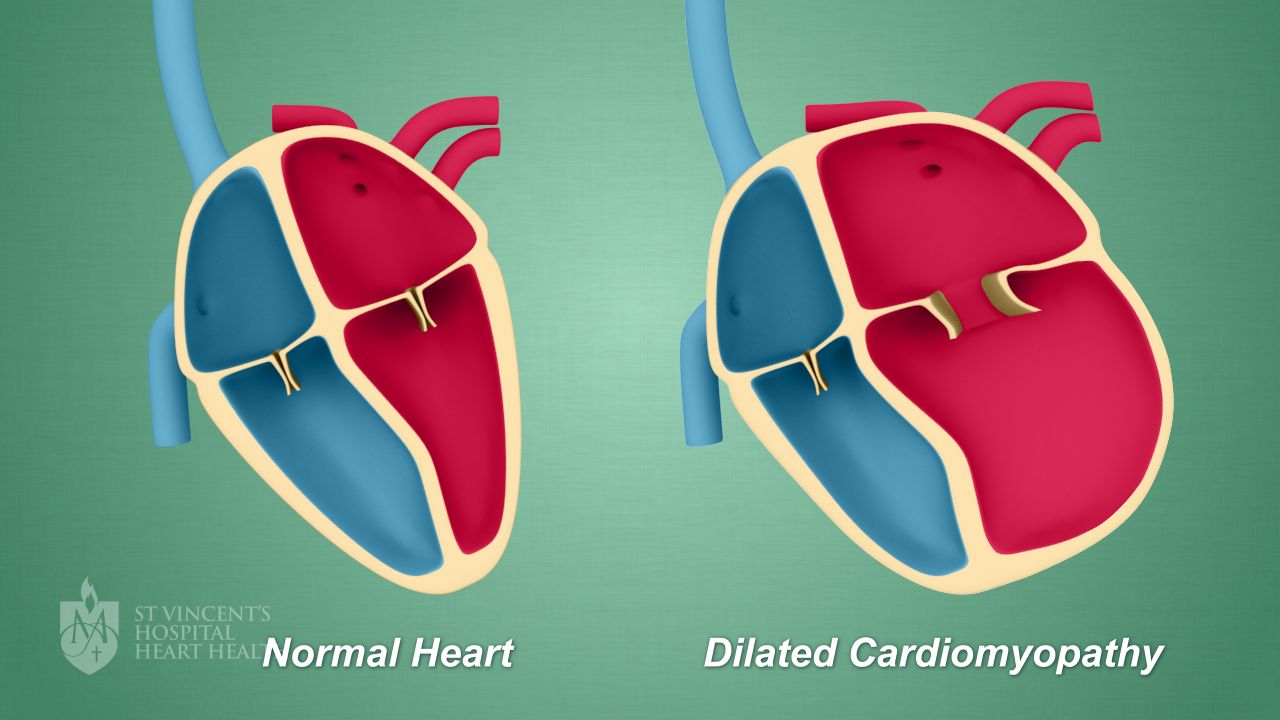
- Dilated cardiomyopathy - when the heart’s chambers become enlarged and weaken
- Hypertrophic cardiomyopathy “HOCM” – when the heart muscle enlarges and thickens, making the hearts chambers narrow. This makes it harder for the heart to pump blood
- Restrictive cardiomyopathy – when the hearts chambers become stiff and rigid without the walls thickening. This means that the hearts chambers are not able to relax and fill with enough blood to pump
- Arrhythmogenic right ventricular cardiomyopathy “ARVC” – when the muscle tissue in the right ventricle is replaced with waxy or fibrous tissue. This can disrupt the hearts electrical system and cause abnormal heart rhythms – called arrhythmias.
- Takotsubo cardiomyopathy – when the heart muscle becomes suddenly stunned or weakened. It mostly occurs following severe emotional or physical stress. The condition is temporary and most people recover within two months.
This image below is an example of dilated cardiomyopathy.
What are the causes of cardiomyopathy?
Cardiomyopathy can be inherited or it can develop from other diseases or factors. Sometimes the cause of cardiomyopathy is idiopathic- not known.
Some causes of cardiomyopathy are:
- Inherited – the gene for the disease is passed on to you from your parents
- Hypertension – high blood pressure
- Alcohol – in large amounts
- Peripartum – during or after pregnancy
- Coronary artery disease – a narrowing of the hearts blood vessels
- Drugs – such as cocaine and amphetamines
- Radiation and chemotherapy - common treatments for cancer
- Other diseases – such as diabetes, sarcoidosis
What are the signs and symptoms of cardiomyopathy?
Not everyone with cardiomyopathy experiences signs and symptoms - particularly in the early stages of the disease. When cardiomyopathy worsens, signs and symptoms of heart failure usually occur including swollen feet and ankles, shortness of breath and tiredness.
You can learn more about heart failure here. Other signs and symptoms may include chest pain, heart murmurs, arrhythmias and dizziness.
What are the possible tests to diagnose cardiomyopathy?
Your doctor will ask you about your symptoms and your medical history, and complete an examination of your heart and lungs, before ordering tests. You may need one or more of the following tests:
- Blood tests – to check how your heart and other organs are responding
- Chest Xray - to check your heart’s size and find out if there is any fluid in your lungs
- Electrocardiogram “ECG” – an electrical recording of your heart’s action
- Holter monitor – to record the heart’s rhythm continuously for 24 hours
- Echocardiogram – an ultrasound of your heart to look at how your heart pumps blood, check your blood flow and see how well your heart’s valves are working
- Stress test – to see how well your heart handles exercise
- Coronary angiogram - to check your blood flow through your coronary arteries. These are the fuel lines that carry blood to the heart muscle
- Cardiac biopsy – to analyse a small piece of heart muscle
What are the possible treatments for cardiomyopathy?
The aim of your treatment will be to improve your symptoms and quality of life, treat any underlying causes of your cardiomyopathy and manage your condition. Treatments for cardiomyopathy include:
What is the future plan if you have cardiomyopathy?
If you have cardiomyopathy, you can take steps to look after your heart. Your medical team will give you guidance and instructions on how to manage your condition and live a healthy life, including:
- Following your dedicated treatment plan – always take your medicines, continue to make healthy lifestyle changes, stay active, and go to your regular medical appointments
- Knowing when to seek help – if something doesn’t feel right, always contact your doctor or cardiac rehabilitation team
- See a dedicated cardiac rehabilitation service or nurse – a team of health professionals can teach you about how to best manage and monitor your condition