Heart Transplant
A heart transplant is surgery to replace your heart with a donor’s heart.
What is a heart transplant?
Why do I need a heart transplant?
What are the risks of having a heart transplant?
How do I prepare for a heart transplant?
What happens during a heart transplant?
What happens after a heart transplant?
What is a heart transplant?
A heart transplant is surgery to replace your heart with a donor’s heart. A heart will be donated to you from a person who has recently passed away and whose family have agreed to donate their heart.
Why do I need a heart transplant?
You may be considered for a heart transplant if you have been diagnosed with end stage heart failure and need life-saving treatment. ‘End stage’ means your heart disease is very severe; you’ve tried all other available treatments, yet they haven’t been able to help. If you have end stage heart failure, you have probably been in and out of hospital many times and have tried different treatments such as:
There is very specific criteria for heart transplant surgery, and not everyone who has end stage heart disease will be eligible for heart transplantation. If you meet the criteria, your medical team will help you understand what’s involved in this major surgical procedure so you can be certain that you really do want to go ahead.
What are the risks of having a heart transplant?
A heart transplant can save your life when all other procedures haven’t helped, but there are serious risks to be aware of. The specific risks associated with heart transplant surgery include:
- Donor heart rejection – when your body considers the donor heart a foreign object and doesn’t accept it
- Cardiac Allograft Vasculopathy (CAV) – when the walls of your coronary arteries in your new heart become thick, hard and less stretchy
- Primary graft dysfunction – when the new heart isn’t able to function, shortly after surgery due to shock or trauma
- Infection – your immune system will be suppressed from medications to prevent organ rejection, making you more susceptible to infections. There are a number of things you can do to reduce the risk of infection. Read the Healthcare Associated Infections Consumer factsheet
- Cancer – you may be at risk of developing forms of cancer from medicines used to suppress the immune system
- Complications from medicines – medicines that prevent rejection, called immunosuppressants, are essential but can cause side effects, such as kidney damage
- Bleeding, stroke and arrhythmias – these can occur during and after surgery
- Ongoing complications – not following your recommended lifelong care plan can increase your risk of complications
It is common for patients to experience delirium following heart transplant surgery. Delirium can be managed by your transplant team, especially if it is detected early.
We encourage you to watch the video below to learn more about delirium and understand how your family is an important part of the team.
These types of risks affect everyone individually - so some people may be more at risk than others. Your doctor will discuss all of the risks with you in detail before you agree to the surgery - and if you do agree, you’ll be asked to sign a consent form. You are also encouraged to discuss any questions or concerns with your medical team.
Remember, at any time, you always have the choice to decide not to proceed with the transplant.
How do I prepare for a heart transplant?
REFERRAL TO A TRANSPLANT DOCTOR
The first step involves being referred to a transplant doctor who will perform a health assessment and review your medical history. Based on this information, the transplant doctor will decide if you are suitable to proceed to the next stage of transplant assessment.
To find out more about what happens at this stage, watch the Introduction to Transplant Assessment Video.
TRANSPLANT ASSESSMENT AND WORK UP
If you are considered suitable for a heart transplant by the transplant doctor, you will need to complete what’s known as ‘the work up assessment for heart transplant suitability’. This includes many different types of tests (the work up process). Some of these tests will be done at hospital and others will be organised by your GP or referring doctor.
During your work up, you will be managed by one of the transplant coordinators. The transplant coordinators will be your main source of communication throughout this stage.
To find out more about transplant assessment and work up, including the criteria for heart transplantation, tests, role of the carer, responsibilities of the patient, and what happens after the tests have been completed, watch the Heart Transplant Assessment Video.
Your medical team will review your medical history, test results, social history and psychological tests. Doing this helps your team to predict where and how you might need support during and after your surgery. For more information about heart transplantation, read our Transplant Information Manual.
You may also find answers to common questions about transplantation in our Heart and/or Lung Transplant Listing Information Booklet - for patients, family, carers and friends.
It is important to realise that going through the work up process does not mean that you will be listed for transplant. Sometimes the work up tests and consultations may highlight problems that may mean you are not suitable for transplant due to a high risk of not having a good outcome.
Vaccinations
Our team recommends you read the Vaccination Guidelines for Pre & Post Heart & Lung Transplant which outline the types of vaccines and their administration schedule.
WAITING LIST
If you are approved for transplant surgery, the final decision to be placed on the transplant list is up to you. If you agree to be activated on the transplant waiting list, you'll need to sign a consent form and wait for a suitable donor.
Your team will see you regularly to monitor your health, and you’ll need to keep your phone with you all the time so you can be notified when a donor becomes available.
We encourage to you watch the Activation on the Transplant Waitlist Video which outlines the waiting times for a transplant, your roles and responsibilities whilst on the waitlist, what to expect whilst on the waitlist and when to contact the transplant team.
Waiting for your heart transplant can be a stressful time, but you will always have the full support of your medical team, as well as friends and family, to help you during this challenging time. Our Dealing with a Transplant book is also a useful resource during this time. You are encouraged to to discuss any questions or concerns with the transplant team.
Transplant social workers provide education and support to patients, families and caregivers throughout the transplant process. To find out more about the role of the transplant social worker, and how they can support you, watch this video below.
TIME FOR TRANSPLANT
When you receive a call to come in for the heart transplant, you will need to move quickly to arrive at the hospital and be ready in time for theatre. Many calls happen after hours, but you need to be prepared to go to hospital at any time of the day or night.
As soon as you know you need to go to the hospital, you’ll need to begin fasting. It’s also important that you keep your mobile phone with you at all times until you go into surgery. When you arrive at the hospital, you’ll be quickly prepared for surgery. This includes:
- Chest X-rays
- Blood tests
- Having your chest shaved
- Showering
- Wearing a hospital gown
- You will also be given some medications to prepare your body for the surgery.
Your family can stay with you until you arrive at the operating theatre, and then they’ll be asked to wait in the ICU waiting room until you come out of the theatre. It’s important to be aware that you could also have one or more ‘false alarms’ - meaning your transplant doesn’t end up going ahead. This can happen if the medical team find out that the donor heart isn’t suitable for you.
Watch the "What to do when you get the call for a transplant" video below to help you prepare.
What happens during a heart transplant?
Your heart transplant surgery will be performed under general anaesthetic. You will be given medications before your surgery to relax and make you fall asleep. You will not be aware of what happens during the surgery. After you fall asleep, your doctor will:
- Make an incision down the centre of your chest - to open the rib cage and access your heart
- Connect you to a heart lung bypass machine - which pumps blood through your body while your heart is being operated on
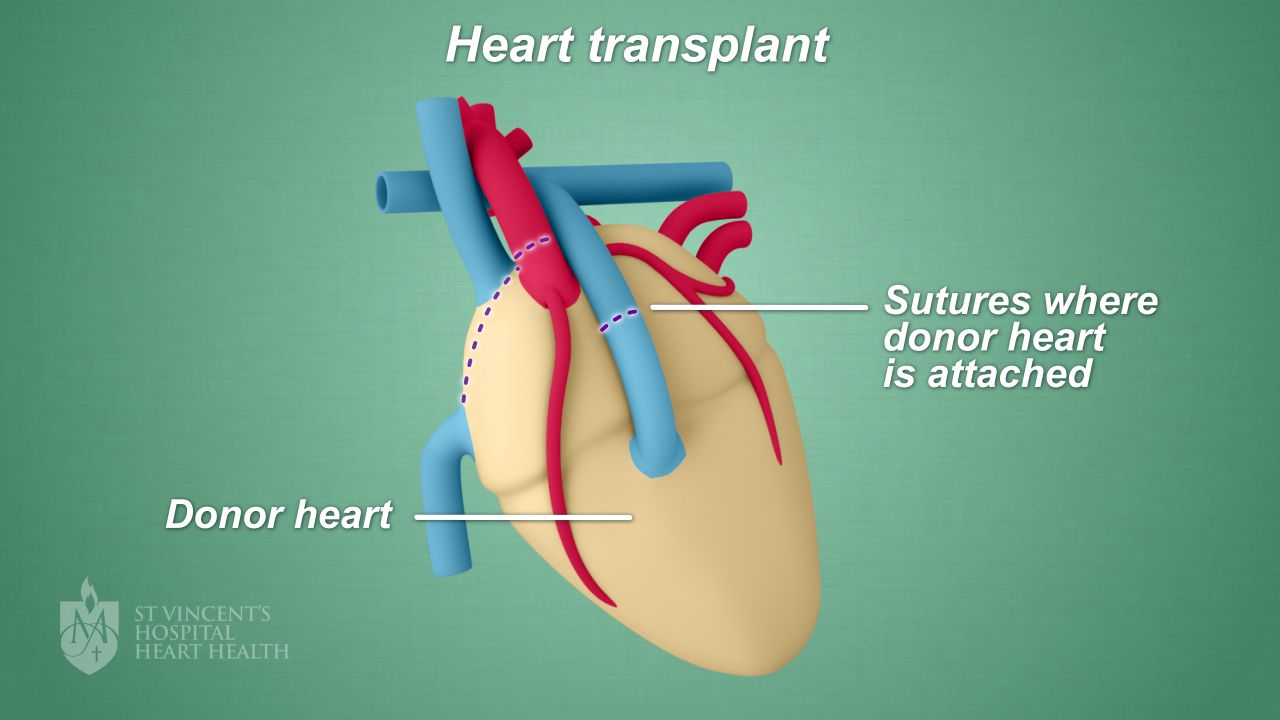
- Remove your diseased heart - and sew the donor heart into place [see image below]
- Connect your new donor heart to temporary pacing wires - to temporarily control the heartbeat
- Give you immunosuppressant medication - to prevent your body from rejecting the donor heart
The image below shows where the donor heart is sewn in place.
The surgery will take about four to six hours.
What happens after a heart transplant?
After your heart transplant surgery, you will be transferred to the Intensive Care Unit (ICU), and you’ll stay there until you have recovered from your operation and become stable. When you first wake up, you may feel drowsy and you’ll have a breathing tube in your mouth. You’ll also be given pain medication orally as well as through an IV cannula into a vein.
Below, you can watch an animation explaining what happens after heart transplant surgery.
Your family and support team, who will have been waiting for you in ICU, can visit you as soon as you are stable. When you’re ready to leave the ICU, you will go to a hospital room on a cardiac ward for one or two weeks. There, you’ll be seen regularly by specially trained medical and nursing staff, dieticians, pharmacists, physiotherapists and social workers. You’ll also have regular blood tests, chest X-rays and ECGs.
Even if you did not have diabetes before, you may develop diabetes after your heart transplant. Diabetes can occur as a side effect from the medication, called steroids, you need to take to prevent rejection of your new heart.
Watch the video below to learn more about diabetes after your heart transplant.
The St Vincent's Hospital Heart and Lung Clinic has a variety of resources, including online and telehealth services, to support transplant recipients throughout their recovery. Visit the Heart Lung Clinic Transplant Services page to find out more.
Below, you can also watch a video demonstrating how to look after your breastbone following heart surgery.
You’ll be able to return home around 2-3 weeks after your surgery, depending on how well you’re recovering. Your medical team will give you detailed instructions on how to recover from your surgery after you have left the hospital; this includes attending regular medical appointments and having frequent heart biopsies for three months after your heart transplant. The heart biopsies will identify if your body’s immune system is accepting your new heart. You’ll also be taught how to:
Recovering from heart transplant surgery requires complete commitment from you and your family or support network. You and the transplant team will work together to protect your new heart.
This means that you need to attend all of your scheduled appointments and a transplant rehabilitation program, and follow the health and lifestyle advice your doctor gives you.
As long as you continue to follow your transplant team’s advice and take your medications, you can be physically and socially active, return to work and have a good quality of life after your successful heart transplant.